How Psilocybin Can Help Treat End-of-Life Anxiety
For many with terminal illness, facing mortality can be one of the most profound and challenging experiences a person endures, sometimes even more so than the physical pain or limitations of the illness. It can result in an overwhelming fear of death, known as end-of-life anxiety or existential distress, which not only diminishes the quality of life for patients but also for their families and caregivers.
Hospice and palliative care specialists find ways to address this distress with compassion. Coping tools, ranging from relaxation practices to antidepressants, can help. And recent research into psychedelic-assisted therapy for end-of-life care is showing increasing promise in creating lasting peace for those with terminal illness.
Defining Existential Distress in Terminal Illness
End-of-life anxiety often manifests as existential distress, a psychological and spiritual pain that arises when a person confronts their own mortality. Patients may experience:
- Fear of ceasing to exist
- Loss of meaning or purpose
- Grief over unfinished relationships or regrets
- Isolation from others or from life itself
Studies by Holland et al., 2013 and others estimate that up to 50% of terminally ill patients may experience significant existential or death-related anxiety, creating a negative feedback loop of rigid thought patterns that can reduce pain tolerance and amplify their suffering.
Many patients express a longing not just for symptom relief, but for a sense of peace, purpose, and connection as they approach death. Traditional palliative care approaches, such as antidepressants, talk therapy, occupational therapy, or spiritual counseling, can help, but sometimes fall short in addressing the psychological and existential aspects of terminal illness.
Psilocybin: A New Paradigm for End-of-Life Care
After decades of prohibition, psilocybin, a naturally occurring psychedelic compound found in specific species of mushrooms, has shown promise in helping terminally ill patients find meaning and acceptance as they grapple with the end of their lives.
Research says…
- As shown by Ross et al., 2016, psilocybin in particular has drawn attention for its ability to induce profound shifts in consciousness that can create lasting relief from end-of-life psychological suffering, including a renewed appreciation for life.
- Clinical studies at major institutions like Johns Hopkins and NYU Langone, and prominent organizations such as Sunstone Therapies, have shown that psilocybin-assisted therapy can dramatically reduce depression and anxiety in patients with life-threatening cancer, often after just one session.
How Psilocybin Helps to Alleviate Distress
Unlike medications or interventions that only treat symptoms or have a short-term effect, psilocybin treatment combines both the pharmacological and psychotherapeutic approaches for lasting relief. This combination helps patients confront and transform their fear rather than “numb out” by facilitating experiences of deep emotional release, spiritual connection, and acceptance.
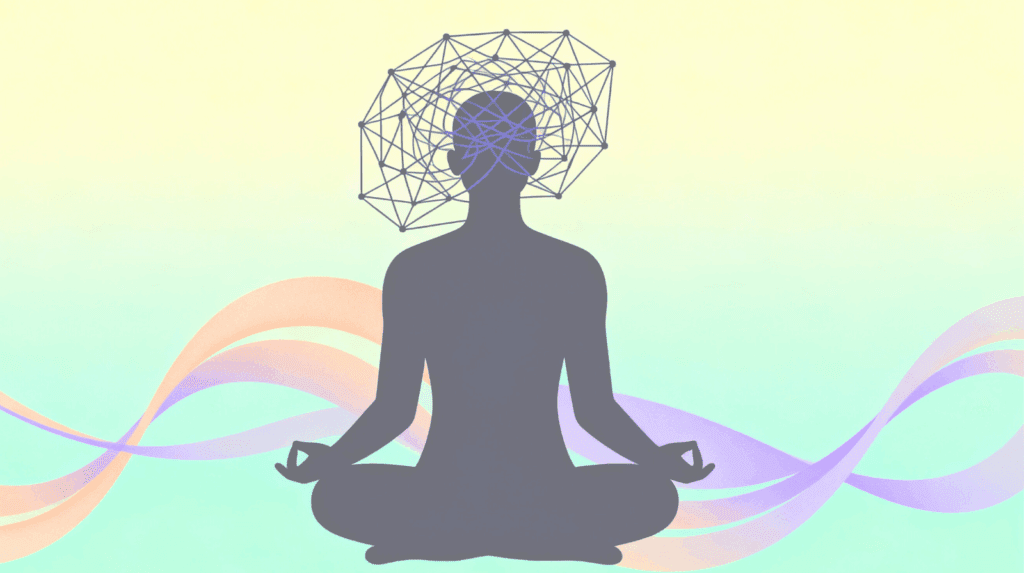
These therapeutic benefits are in part due to psilocybin’s varied effects in the brain. Because psilocybin is structurally similar to the neurotransmitter serotonin, it can affect specific receptors and areas of the brain that are involved in emotional regulation and self-identity. When psilocybin activates these areas, it greatly affects mental processes. This flurry of activity calms fear centers, scrambles connections, and boosts the brain’s ability to make new connections, strengthens neural growth through neuroplasticity, and reduces activity in areas of the brain related to the sense of self.
In short, it provides a neurobiological reset where the brain’s rigid patterns loosen, the ego quiets down, and patients feel more spiritually and emotionally open. Some patients describe psilocybin sessions as “years of therapy in one day.” This phenomenon has been explored in best-selling books such as How to Change Your Mind and documentary films such as Fantastic Fungi, in which terminally ill patients share their positive experiences. \
Landmark Research & Promising Outcomes
Two pivotal studies conducted in 2016, one at Johns Hopkins University and a parallel one at NYU Langone Medical Center, brought psilocybin therapy for end-of-life anxiety into the scientific spotlight.
Both were randomized, double-blind studies of cancer patients struggling with existential distress, and both found that a single psilocybin session produced profound and sustained psychological benefits. Since the publication of these two landmark papers, more research has been unfolding that supports the original findings.
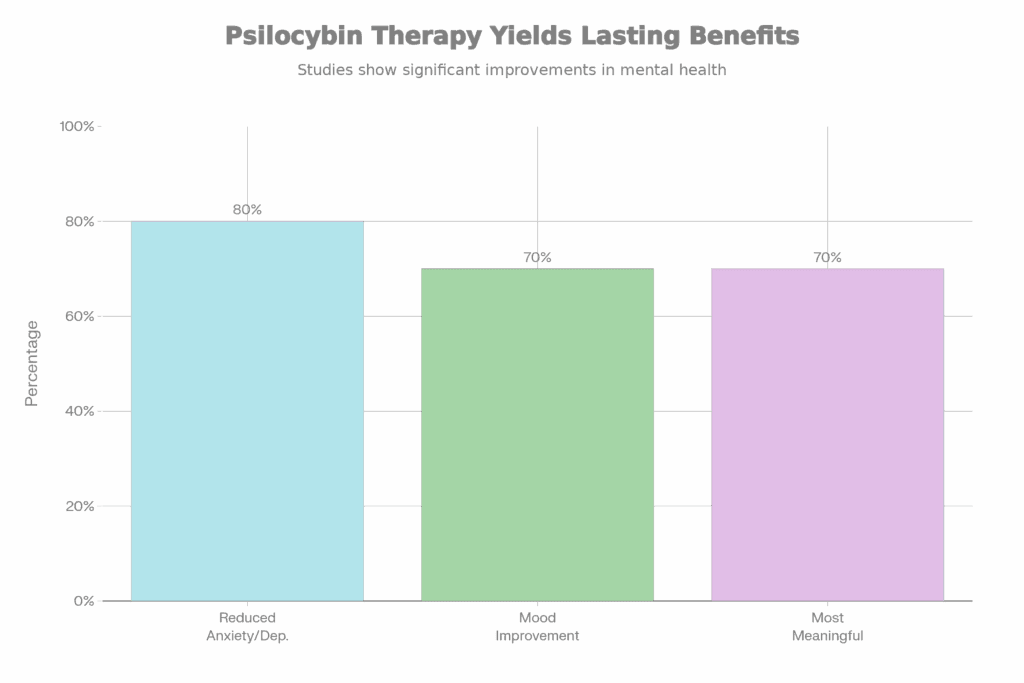
Key Findings: Reduced Anxiety, Depression, and Improved Quality of Life
Both studies emphasized safety and tolerability. Adverse events were rare and transient, with most participants describing the experience as challenging but ultimately healing.
The results:
- 80% of participants in the Johns Hopkins study showed clinically significant reductions in anxiety and depression.
- 70% of NYU participants maintained clinically significant improvements in mood, spiritual well-being, and life satisfaction six months after treatment.
- Participants of both studies described increased life satisfaction, meaning, and acceptance of death.
- 70% of participants reported experiences that rated among the most meaningful of their lives.
The benefits:
- Ego Dissolution: Patients reported feeling “oceanic boundlessness,” a meaningful experience of unity with their surroundings, and temporary reprieve from their daily worries and thought patterns. Some patients found ego-dissolution challenging, but in general, studies such as the one from Johns Hopkins, found that this experience dramatically reduced fear of death and reframed mortality as a transition rather than an end.
- Increased emotional openness and processing: Feelings such as grief, guilt, fear, or regret that may otherwise intensify near the end of life were reduced and transformed. As stated in the NYU study, “psilocybin was associated with improved attitudes and adaptations to death.”
- Fear reduction: Participants described the sessions as mystical or spiritually significant, meaning they evoked a profound sense of interconnectedness, love, and acceptance, which helped patients reframe their own deaths within a larger continuum. Some described the experience as comparable to the birth of a child or the death of a parent.
Johns Hopkins’ lead researcher, Roland Griffiths, who himself was diagnosed with a terminal illness, has said of his own psychedelic treatment, “My experience during the [psychedelic] session felt informative and validating: I would indeed eventually die from the cancer. There was no trace of fear or anxiety, but there was something exquisitely beautiful, uplifting, and deeply meaningful about the process.”
Durability of Effects: Sustained Benefits Over Time
Follow-up studies by NYU and others by Johns Hopkins confirm that the antidepressant and anxiolytic effects of psilocybin can persist for months or even years. Patients often report enduring changes in their feelings about death and dying.
Ethical Considerations and the Future of Psilocybin in Palliative Care
Patient Autonomy and Informed Consent
Studies have shown that psychedelic palliative care patients fear potential mental distress, providers who aren’t adequately trained, and exploitation. Because psilocybin induces powerful altered states, ensuring informed consent is essential. Other key considerations include: screening, support with medical oversight, and integrative care to make patients feel more comfortable.
Accessibility and Training for Therapists
It has also been noted that access to therapy sessions comes with socioeconomic barriers. Some clinics have high rates for psychedelic palliative care or require travel for the legal use of psilocybin, which is more difficult for geriatric or sick populations. Also, access and research are often biased toward white, financially privileged individuals.
However, as laws change and the field of palliative care evolves, accessibility and research are also expanding. Training for therapists who are adept at both clinical care and spiritual presence will allow them to hold space for such profound journeys.
Expanding Access: Clinical Trials and Policy Changes
Psilocybin remains a Schedule I substance in many countries, but momentum in drug reform is growing. Though the FDA rejected the use of MDMA for therapy in 2024, stating more research was needed, it has granted psilocybin and psilocybin analogs “breakthrough therapy” designations for depression over the years.
Clinicians and researchers remain undaunted as promising results from pilot studies in psychedelic palliative care have led to larger, multi-center trials. This includes phase 2 and phase 3 studies currently underway to further investigate efficacy, safety, and optimal dosing in more diverse palliative care populations, with more studies on the horizon.
If approved, psilocybin could soon become an integral tool in helping patients die with dignity, peace, and connection.
Frequently Asked Questions
Is psilocybin legal for end-of-life anxiety?
Currently, psilocybin is illegal for general use in most countries, though reform is happening. A few countries, such as Jamaica, where Beckley retreats are held, do not regulate psilocybin use. Additionally, some U.S. cities and states have decriminalized it, while others, such as Oregon and Denver, have legalized it for use in treatment centers and offer limited compassionate-use programs for palliative care.
How safe is psilocybin for terminally ill patients?
While more research is necessary to understand dosing and other side effects of psilocybin for sensitive populations, when administered in controlled settings with trained therapists, psilocybin is considered physiologically safe. Any psychological risks, such as temporary anxiety or confusion, are mitigated through preparation and support.
What are the benefits of psilocybin for death anxiety?
Psilocybin can reduce fear, depression, and existential distress, while fostering acceptance, peace, and a sense of connection that helps patients face death with calm and meaning.
Will psilocybin change my personality at the end of life?
Rather than changing personality, psilocybin often helps patients reconnect with their authentic selves, reducing emotional rigidity and deepening their compassion and gratitude for life.
How does psilocybin-assisted therapy work in hospice care?
In hospice settings, psilocybin therapy may involve collaboration between palliative care providers, therapists, and spiritual counselors to ensure holistic support before, during, and after the session. Though legally, there are only a few places where this type of care can take place.
Sources
- Holland JC, Andersen B, Breitbart WS, et al. Distress Management. J Natl Compr Canc Netw. 2013;11(2):190-209. doi:10.6004/jnccn.2013.0027
- Hermann Faller et al. Effects of Psycho-Oncologic Interventions on Emotional Distress and Quality of Life in Adult Patients With Cancer: Systematic Review and Meta-Analysis. J Clin Oncol 31, 782-793(2013). DOI:10.1200/JCO.2011.40.8922
- Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165-1180. doi:10.1177/0269881116675512
- Agrawal M, Richards W, Beaussant Y, et al. Psilocybin-assisted group therapy in patients with cancer diagnosed with a major depressive disorder. Cancer. 2024;130(7): 1137-1146. doi:10.1002/cncr.35010
- Watts, R., Day, C., Krzanowski, J., Nutt, D., & Carhart-Harris, R. Patients’ accounts of increased “connectedness” and “acceptance” after psilocybin for treatment-resistant depression. Journal of Humanistic Psychology. 2017;57(5), 520–564. doi:10.1177/0022167817709585
- Siegel, J.S., Subramanian, S., Perry, D. et al. Psilocybin desynchronizes the human brain. Nature. 2024;632,131–138. Doi:10.1038/s41586-024-07624-5
- R.L. Carhart-Harris, D. Erritzoe, T. Williams, J.M. Stone, L.J. Reed, A. Colasanti, R.J. Tyacke, R. Leech, A.L. Malizia, K. Murphy, P. Hobden, J. Evans, A. Feilding, R.G. Wise, & D.J. Nutt, Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin, Proc. Natl. Acad. Sci. U.S.A. 109 (6) 2138-2143, https://doi.org/10.1073/pnas.1119598109 (2012).
- MacLean KA, Johnson MW, Griffiths RR. Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J Psychopharmacol. 2011;25(11):1453-1461. doi:10.1177/0269881111420188.
- Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-1197. doi:10.1177/0269881116675513
- Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology (Berl). 2006;187(3):268-292. doi:10.1007/s00213-006-0457-5
- Yaden, David B, and Roland R Griffiths. The Subjective Effects of Psychedelics Are Necessary for Their Enduring Therapeutic Effects. ACS pharmacology & translational science vol. 4,2 568-572. 2020. Doi:10.1021/acsptsci.0c00194
- Agin-Liebes GI, Malone T, Yalch MM, et al. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Journal of Psychopharmacology. 2020;34(2):155-166. doi:10.1177/0269881119897615
- Sweeney MM, Nayak S, Hurwitz ES, Mitchell LN, Swift TC, et al. (2022) Comparison of psychedelic and near-death or other non-ordinary experiences in changing attitudes about death and dying. PLOS ONE 17(8): e0271926. https://doi.org/10.1371/journal.pone.0271926
- Julia Ruixi Wang, et al. “Palliative Care Patients’ Attitudes and Openness towards Psilocybin-Assisted Psychotherapy for Existential Distress.” Frontiers in Psychiatry, vol. 15, 18 Apr. 2024, https://doi.org/10.3389/fpsyt.2024.1301960.
- Whinkin E, Opalka M, Watters C, Jaffe A, Aggarwal S. Psilocybin in Palliative Care: An Update. Curr Geriatr Rep. 2023;12(2):50-59. doi:10.1007/s13670-023-00383-7
- Nicole Cornish, Tara Coles, M. Jennifer Cheng, Claudia Ruiz Sotomayor, Aaron Wolfgang, Christopher Spevak. Cleveland Clinic Journal of Medicine. 2025; 92 (4) 248-25.; DOI: 10.3949/ccjm.92a.24100